 Telehealth is an innovative health care approach amid the COVID-19 pandemic. Organizations are using it to respond to COVID-19 by monitoring symptoms and caring for inpatients–as well as providing regular health care services to patients in their homes due to self-quarantine or stay-at-home requirements.
Telehealth is an innovative health care approach amid the COVID-19 pandemic. Organizations are using it to respond to COVID-19 by monitoring symptoms and caring for inpatients–as well as providing regular health care services to patients in their homes due to self-quarantine or stay-at-home requirements.
The president’s administration expanded the telehealth benefits. This prompted the Center for Medicare and Medicaid Services (CMS) to expand the waiver authority on March 17, 2020, by indicating that certain limitations related to telehealth wouldn’t be enforced.
Under the 1135 waiver, telehealth benefits are expanded for Medicare beneficiaries to allow for telehealth visits with patients who can now be located in either rural or urban areas and other non-health care type sites such as the patient’s home during the COVID-19 outbreak.
With the expansion, however, there are still elements to consider in order to comply and receive payment. Learn more about those parameters below.
Qualified Providers
According to CMS, an individual is qualified to provide and bill for the services if they are:
- A physician
- A nurse practitioner (NP)
- A physician assistant (PA)
- A certified nurse-midwife
Other practitioners may be able to furnish services within their scope of practice and consistent with Medicare benefit rules that apply to all services such as:
- A clinical nurse specialist (CNS)
- A certified registered nurse anesthetics (CRNA)
- A clinical psychologist (CP)
- A clinical social worker (CSW)
- Registered dieticians (RD)
Organizations should also validate the scope of licensing regulations of their state as they engage providers to assist patients.
Expansion of Services
CMS released an interim final rule which will expand the number of services covered by CMS to approximately 80 as of March 30, 2020. The interim rule lists the additional services, but hasn’t updated the definitions related to qualified providers.
Health care organizations should assess the additional services and determine which qualified provider can perform the services based on the scope of licensing.
Covered Services
There are three types of services covered by Medicare as follows.
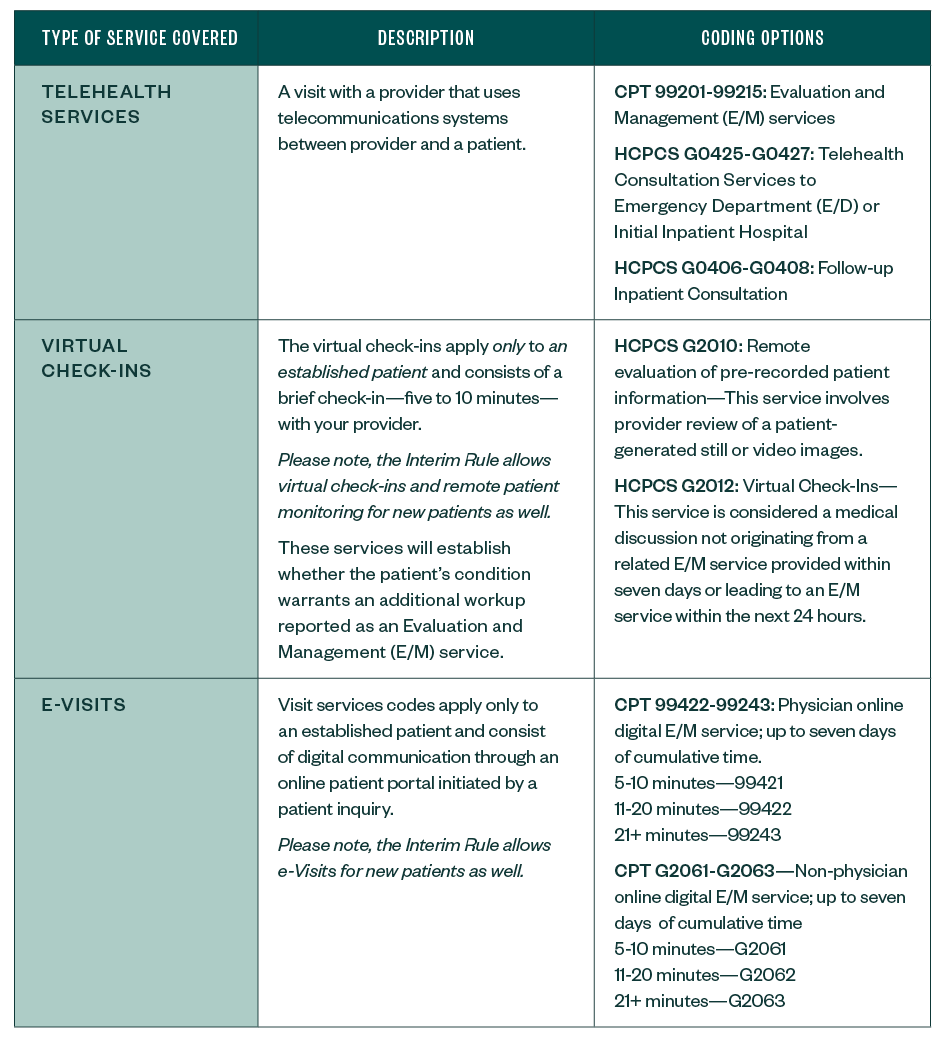
Additional Services allowed for COVID-19 pandemic effective March 1, 2020 can be found on the CMS website.
Documentation
Documentation requirements have not changed due to the waiver, other than the mode of how to provide the services and location of provider—the distant site–and location of the patient—originating site.
However, there are some important elements to remember as noted below.
New Patient Appointments
- For an initial appointment with a new patient, the provider must review the patient’s relevant medical history and any available medical records with the patient before initiating the delivery of the service.
- Confirm the type of visit is for a new patient by confirming the patient hasn’t received services by the provider or provider group specialty within the three years prior.
- Include in the documentation that the patient is new.
Established Patient Appointments
- For existing provider-patient relationships, the provider must review the patient’s medical history and any available medical records with the patient during the service.
- Include in the documentation that the patient is an established patient.
Virtual Check-In Visits
- For virtual check-in visits, ensure the service isn’t related to a prior E/M visit within the past seven days or leading to an E/M service within 24 hours.
- An organization should identify a mechanism to assist the provider in validating this prior to the telehealth visit.
Telehealth E-Visits
- When completing telehealth E-Visits, include language in the encounter note that the E-Visit Service was initiated by a patient inquiry.
- Prior to the telehealth visit, verify that the patient is an established patient of the provider or provider group specialty.
- Prior to the telehealth visit, document in the encounter note any prior conversations with the patient in regards to education on the availability of the E-Visit Service.
- Each organization should have controls in place to ensure the correct CPT/HCPCS code is selected based on the type of provider—physician or non-physician.
Best Practices
Health care organizations will be faced with ensuring patients are comfortable with the new technology and also protecting against individuals who wish to take advantage of them.
Below is a summary of best practices for telehealth encounters.
Verification
Providers should properly identify the patient using, at a minimum:
- Patient’s name
- Date of birth (DOB)
- Other identification based on the organization’s Health Insurance Portability and Accountability Act (HIPAA) identification policy
Communication
A provider should always disclose and validate:
- Provider’s identity and credentials, such as license, title, and, if applicable, specialty and board certifications
- Location of the provider rendering services via telehealth
The provider should also obtain the location of the patient, and both the location of the provider and patient should be noted in the record.
A statement in the encounter note identifying the service was provided by telecommunication means, such as telephone or online platforms like Skype, should be included as well.
Delivery of Service
If the patient must be seen by a clinician based up on the findings from the telehealth provider, then the provider must inform the patient of how they can see a clinician in-person in the event of an emergency or as otherwise needed.
An organization may want to consider a mechanism that will allow the telehealth provider to create a notification about the patient symptoms and reason for the in-person appointment to the clinician or facility.
Prior to each telehealth appointment, the provider must ensure they’re able to deliver service to the same standard of care using telehealth as is applicable to the delivery of services in person.
Telehealth services must be in compliance with all of the following:
- Licensure regulations and requirements
- Programmatic regulations
- Performance specifications related to the service such as accessibility and communication access.
If the provider can’t meet this standard of care or other requirements, the provider must direct the patient to seek in-person care. The provider must make this determination prior to the delivery of each service.
Confidentiality and Security
To the extent feasible, providers must ensure the same rights to confidentiality and security as provided in face-to-face services.
- Providers must inform members of any relevant privacy considerations. An example would be to ask if the patient is able to have a confidential discussion.
- Organizations and providers must follow the same consent and patient information protocol consistent with those followed during in person visits.
- At a minimum, obtain a verbal consent and document the consent in the medical record. Consider having the consent sent and received from the patient prior to the telehealth visit.
We’re Here to Help
The CMS has also provided a tool kit, a fact sheet, and a list of frequently asked questions as additional resources.
If you have any questions about how your organization is engaging in telehealth appointments, please contact your Moss Adams professional.